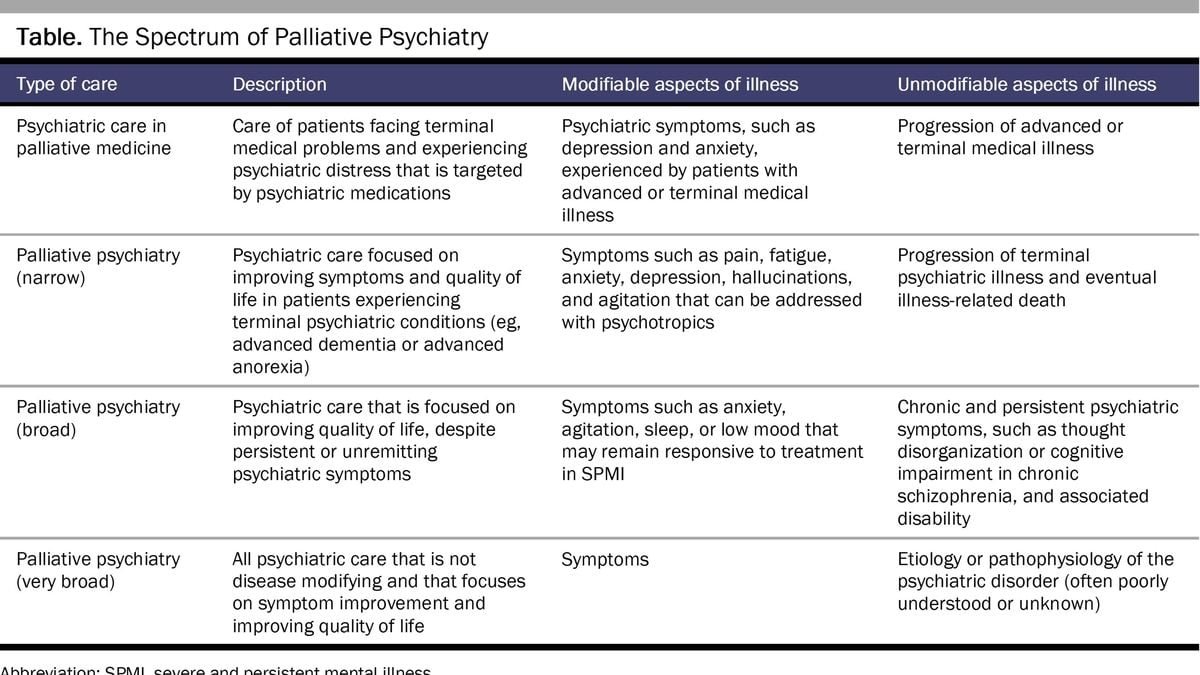
Imagine a realm of healthcare where the focus shifts from relentless battles against symptoms to a compassionate acceptance of living with mental illness, emphasizing quality of life over aggressive interventions. This is the essence of palliative psychiatry, a pioneering approach that extends the principles of palliative care—traditionally reserved for the terminally ill—to those grappling with severe and enduring mental disorders. As we explore this innovative frontier, we uncover the potential of palliative psychiatry to offer solace, dignity, and a fuller life to individuals for whom conventional treatments have reached their limits.
A Compassionate Approach to Mental Health
The inception of palliative psychiatry draws inspiration from Cicely Saunders’ groundbreaking work in hospice care and the concept of “total pain.” It acknowledges the multifaceted suffering of patients with serious mental illnesses, including schizophrenia, bipolar disorder, and severe depression, whose lives are often curtained by the shadow of unremittent symptoms. Through palliative psychiatry, an interdisciplinary team of psychiatrists, nurses, social workers, and other healthcare professionals come together to provide a holistic care plan focused on easing emotional pain and fostering acceptance of life’s limitations.
In Canada, the discussion around Medical Aid in Dying (MAiD) for individuals with mental illness further illuminates the importance of adopting a palliative approach within psychiatry. This development underscores the ethical imperative to explore every possible avenue of care that honors the dignity and complexity of human suffering beyond mere physical ailments.
Challenges and Ethical Debates
Despite its promising outlook, palliative psychiatry faces skepticism within the mental health community, partly due to its association with end-of-life care. Critics argue that such an approach could diminish efforts to find effective treatments, potentially leading to a form of therapeutic nihilism. However, proponents emphasize that palliative psychiatry is not about giving up on patients but rather about offering a more nuanced, patient-centered form of care that acknowledges when traditional interventions may no longer be beneficial.
The introduction of MAiD for mental illness has sparked ethical debates regarding the criteria and safeguards necessary to ensure it is a genuine choice for patients whose suffering is intolerable and incurable by other means. This conversation highlights the critical need for comprehensive palliative care frameworks in psychiatry, which can provide an alternative avenue for relief and support for those with severe mental illnesses.
Looking Forward: The Future of Palliative Psychiatry
The evolution of palliative psychiatry represents a significant paradigm shift towards a more compassionate, patient-centered approach in mental health care. It challenges us to reconsider our definitions of recovery and success in the treatment of severe mental disorders. By incorporating advanced care planning and emphasizing the importance of patient autonomy and dignity, palliative psychiatry seeks to bridge the gap in care for those who have long been marginalized within the healthcare system.
As research and practice in this field continue to grow, it is crucial to foster dialogue among healthcare professionals, patients, and families to ensure that palliative psychiatry develops in a way that truly meets the needs of those it aims to serve. The journey towards mainstreaming palliative psychiatry may be fraught with challenges, but its potential to enhance the quality of life for individuals with serious mental illnesses offers a beacon of hope and a reminder of the profound impact of compassionate care.